When Hurricane Helene damaged Baxter International’s primary intravenous fluid factory, it sparked a national shortage, impacting hospitals nationwide. Pediatric anesthesiologists like me are already choosing how to adjust the care we provide, knowing we may run low on specialized fluids.

Across the country, pharmacists are scrambling to deal with this critical shortage, using their incredible skills to figure out how to continue to offer routine treatments like hydration, hemodialysis (kidney failure treatment), and medications that need to be diluted in sterile saline. So many of the medicines we use every day, such as antibiotics, chemotherapy, and TPN, require access to a consistent, safe supply of sterile fluids.
While natural disasters often disrupt supply chains, the effects we’re witnessing highlight deeper, systemic issues rooted in geography, politics, and the impacts of capitalism on healthcare access.
The Immediate Crisis
Hurricane Helene recently struck the southeastern U.S., damaging Baxter International's primary manufacturing plant for IV fluids in North Carolina. This facility supplies around 60% of the IV fluids used in the U.S., and its temporary shutdown has exacerbated pre-existing shortages, affecting saline, dextrose solutions, and sterile water—all staples in hospitals. Healthcare providers are now forced to conserve supplies, postponing some elective surgeries and shifting patients to oral hydration or alternative methods when possible. However, some patients are not able to use alternatives, meaning their care is especially precarious.
On Wednesday, the Food and Drug Administration (FDA) authorized temporary imports of certain IV products from Canada, China, Ireland and the U.K.
In an effort to prevent hoarding, Baxter is limiting how much of its IV fluids customers like hospitals can buy. They are trying to ensure equitable access to the available supply. It’s also trying to increase manufacturing at its other facilities to bridge the gap.

Thankfully, when Hurricane Milton hit Florida, it spared another primary manufacturing site for IV fluids in Daytona Beach.
A Recurring Problem
This isn’t the first time a hurricane has caused supply chain disruptions. A similar situation unfolded after Hurricane Maria struck Puerto Rico in 2017, leading to nationwide IV fluid shortages. While many Americans don’t realize Puerto Rico is part of America, the nation had a wake-up call when it became clear we rely on pharmaceuticals produced on the island. Puerto Rico’s Baxter facilities were major producers of IV solutions at the time, and the damage from that storm revealed the fragility of the U.S. medical supply chain.
Puerto Rico’s experience highlights a glaring issue: how tax incentives for corporations and low wages for workers lead to the centralization of critical medical manufacturing. In the late 1960s and 1970s, pharmaceutical companies flocked to Puerto Rico to take advantage of the now-expired federal tax incentive known as Section 936. This incentive, valid through 1996, allowed U.S.-based manufacturers to send all profits from local plants to stateside parent plants without paying federal taxes. Such businesses also capitalized on low wages in Puerto Rico. Puerto Ricans are twice as poor as people in the poorest American states and three times as poor as the average American.
The same types of incentives drive major businesses to consolidate manufacturing in places like North Carolina and Florida. North Carolina boasts the lowest corporate tax rate in the US and courts businesses to move there. The Sunshine State charges no corporate income tax on limited partnerships or on subchapter corporations.
In a capitalist-driven healthcare system, companies are incentivized to consolidate production in tax-friendly locales to reduce costs. This business model, while profitable, leaves the system susceptible to devastating bottlenecks when a natural disaster strikes. When a single location is responsible for such a large portion of the nation's supply, the ripple effects of its shutdown are felt everywhere, from urban hospitals to rural clinics.
Geography, Politics, and Supply Chain Disparities
Hurricane Helene hit a particularly vital point in the U.S. supply chain. North Carolina houses Baxter's largest facility, and its closure has caused hospitals nationwide to face uneven distribution of the remaining supplies. Larger hospital systems, often with greater buying power, are more capable of securing scarce resources, while smaller or rural hospitals may struggle to meet their patients‘ needs. This unevenness in supply access brings sharp relief to the geographic and economic disparities already in healthcare.
While federal agencies such as the Department of Health and Human Services (HHS) are working to coordinate relief efforts, their ability to manage a crisis of this scale is limited by the privatized nature of healthcare manufacturing. Calls from major medical organizations and government oversight groups to establish more government oversight and stockpiles of critical supplies have been growing louder since Hurricane Maria devastated Puerto Rico, but little has changed in practice. This leaves hospitals dependent on a fragile network of corporate suppliers with little governmental intervention to ensure equity during times of crisis.
A Crisis of Ethics
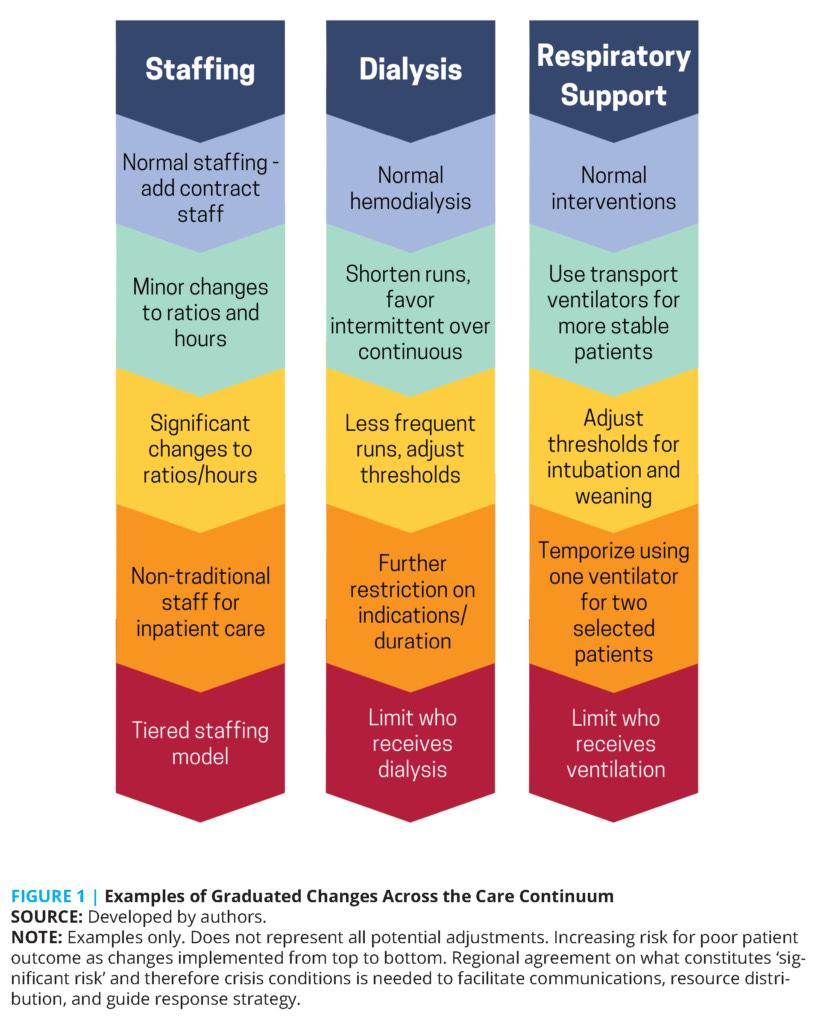
At its core, this crisis is not just a logistical or economic issue—it fuels bioethical dilemmas. Much like fears of ventilator shortages in early in the COVID pandemic, the supply of specific medical resources can lead to rationing.
As an anesthesiologist, the scarcity of IV fluids directly affects my ability to care for patients, who often need fluids to maintain blood pressure while unconscious. Critical care decisions, such as which surgeries to prioritize or which patients should receive limited supplies, risk being dictated by resource availability rather than medical need. These are the kinds of ethical decisions that healthcare professionals dread—choices that feel more like triage in a battlefield than the everyday operations of a modern hospital.
The current situation also reveals how capitalism in healthcare threatens the ethical core of our role as caregivers. In a system where profit maximization often trumps public and individual health, the consolidation of production and the outsourcing of critical medical supplies to disaster-prone regions create vulnerabilities that harm patients. Is it ethical to allow profit-driven decisions to put lives at risk? Why hasn’t the government taken a more active role in safeguarding essential medical supplies? We must grapple with these questions as we face a future where climate change will likely bring more frequent and severe disruptions to global supply chains.
Reforming the Supply Chain
This crisis should serve as yet another wake-up call to reexamine how we manage essential medical supplies. While hospitals and healthcare providers must implement stricter conservation protocols during emergencies, as many are already doing in the wake of Helene, we should not rely on ad hoc rationing schemes. But more broadly, we need systemic reform to ensure our healthcare infrastructure is resilient in natural disasters.
On a national level, policymakers must prioritize creating a more diversified and decentralized medical supply chain. Rather than relying on a handful of manufacturers concentrated in vulnerable regions, we should encourage the development of regional production hubs and create strategic stockpiles of critical medical supplies. No one disaster should threaten the nation’s access to care.
Capitalism in healthcare continues to harm the people - from patients to providers. The profit-driven model makes corporations wealthier while putting the most vulnerable at the greatest risk. These companies are not benevolent and are not motivated to prepare for crises. Greater government oversight and regulation could help prevent shortages like the one we’re experiencing now.
As healthcare professionals, we must advocate for these changes. Preventable shortages should not compromise our ability to care for patients. It is now laid bare that the calls for change after Hurricane Maria were not enough. We must push for the necessary reforms before attention is lost to the next headline.
We deserve a more resilient, ethical healthcare system—one that puts patients before profits and safeguards access to critical supplies in times of need.
Resources
Fluid Shortage Management and Conservation Strategies, American Society of Health-System Pharmacists (ASHP)
IV Bag Shortage Due to Hurricane Helene, USA Today
Hurricane Relief and Baxter's IV Fluid Supply Chain Disruption, Healthcare Dive
Baxter Says Saline Shipments Disrupted in Hurricane-Wracked Puerto Rico, WSJ
Hospitals Conserve IV Fluids Amid Hurricane Helene, NBC News
Milton spares Daytona Beach, Florida, factory that's a critical supplier of IV fluids, ABCNews
The Rise and Fall of Section 936, Teaching for Change
How Hurricane Maria Worsened Puerto Rico’s Health Care Crisis, Commonwealth Fund
Crisis Standards of Care and COVID-19: What Did We Learn? How Do We Ensure Equity? What Should We Do? By John L. Hick, Dan Hanfling, Matthew Wynia, and Eric Toner, National Academy of Medicine, 2021.
IV Fluid Shortages and Elective Hydration Bars During Hurricane Helene, STAT News
Drug shortages: The invisible epidemic, 2018, American College of Surgeons Bulletin
Could Puerto Rico’s Response to Hurricane Maria Help with U.S. Medical Shortages? Milwaukee Journal Sentinel
Hurricane Helene: Baxter's manufacturing recovery in North Carolina, FDA





Excellent article Alyssa.