Be a Strong Link for Immigrant Patients 🔗
Enhance the ethical care of all patients when immigration agents enter hospitals
ICE and CPB agents should be treated like any other hospital visitor - with restricted access.
Healthcare workers:
Does your facility have a plan to protect patients when ICE agents enter care spaces?
Do you know your duties to patients?
Do you know your patient’s rights?
Now is a great time to plan ahead before you’re face-to-face with an ICE agent.

On his first full day in office in his second term as president, Donald Trump rescinded Biden-era guidance against immigration raids in sensitive areas, including elementary and secondary schools, colleges, churches, and hospitals.
Undocumented immigrants have long feared seeking medical care for fear it will lead to deportation. This fear is real, leading patients to delay or avoid needed healthcare.
Both Immigration and Customs Enforcement (ICE) and Customs and Border Protection (CBP) agents can be expected to utilize this increased permission to gather up people in places previously believed to be safer.
The 4th Amendment limits Immigration Enforcement Power
The Fourth Amendment limits ICE and CPB’s powers, but when undocumented people seek medical care, the picture can become complicated and place patients at risk.
“ICE and CBP’s power to enforce immigration law is limited by our constitutional protection against unreasonable search and seizure. Under the Fourth Amendment to the U.S. Constitution, the permissibility of a search depends on whether a person has a reasonable expectation of privacy in the area searched…Your patients thus may be more vulnerable to immigration enforcement actions when they are in areas of your facility that are open to the public than when they’re in areas that are considered private.”
States Diverge on Response
As expected, states already diverge in their response to Trump’s order along partisan lines, leading to state specific challenges for healthcare providers.
California advises healthcare providers not to write down patients' immigration status on bills and medical records. Additionally, healthcare workers should be instructed they do not have to assist federal agents in arrests. In 2023, the University of California updated internal guidance for hospitals.
Florida (May 2023) and Texas (August 2024) require hospitals that receive Medicaid or Children’s Health Insurance Program (CHIP) funding to collect immigration status from patients. Federal law requires that patients’ response will not affect their care and that they cannot be denied emergency care. As Florida’s law is currently written, hospitals must also notify patients that the response will not result in a report to immigration authorities. There is no similar requirement in the Texas law. (In 2013, Arizona attempted and failed to pass a similar law.)
Due to the problem of violence against healthcare workers, a North Carolina law went into effect on October 1, requiring armed police to be present in every emergency department. Such consistent police presence may mean North Carolina healthcare workers and patients are more conditioned to law enforcement presence in hospitals, generally. This presence may also weaken claims under the 4th Amendment.
I have no doubt that the current administration will continue to undercut any protection owed to immigrant patients. As we’ve seen with anti-abortion and anti-trans legislation, legislators know that healthcare workers are powerful agents in protecting patients.
Limiting our ability to act ethically to protect patients will be used against us.
Be A Strong Link, not a Weak Link
Right now, healthcare workers wonder if they are required to answer questions from immigration officials. They may also wonder if they face a penalty if they do not comply with requests for information about patients. Some workers, sympathetic to Trump’s immigration actions, will also wonder if there will be any professional or legal consequences for releasing a patient’s immigration status.
While many healthcare workers are anxious about their immigrant patient’s safety, some healthcare workers are likely to report patients to law enforcement.
HIPAA protections alone are insufficient to protect patient privacy and safety. Yet they are a minimal floor that must be honored regarding privacy. Our sacred duty to protect patients from harm is a much higher, and even more important, standard.
This means that healthcare workers who don’t know their obligations to patients and health systems that don’t provide clear guidance to their employees create easy targets for immigration agents who enter hospitals. Preparation is a major way to prevent healthcare workers from being the weak links in patient care. By preparing healthcare workers with guidance on how to interact (or not) with ICE agents, health systems can decrease the risk of patient and staff intimidation and from inappropriate, unethical, and illegal disclosures of patient information.
Do Not Comply in Advance
Healthcare workers can act as an important line of defense to protect their patients from mistreatment in the hospital. Outside of the Texas and Florida cases mentioned above, healthcare workers have no affirmative legal obligation to ask patients about their immigration status or to document it in the medical record. Healthcare workers have no legal obligation to report patient immigration status to federal authorities. Compliance with agents’ attempts to access clinical spaces and question patients and staff is not required.
However, unprepared healthcare workers may volunteer information to law enforcement when they are not obligated to do so.
Appropriate Barriers to Access
Because ICE does not have an unrestricted legal right to enter patient care areas, hospitals and emergency departments must work now to ensure access is sufficiently controlled to protect the interests of patients.
If a hospital area is closed to the public, it can be closed to ICE. Unless provided specific legal access to a hospital area, then ICE agents should be treated like any other visitor - with restricted access.
ICE and CBP are Visitors in a Hospital Like Everyone Else Who Isn’t a Patient
When approached by a law enforcement agent for access to a patient, always request a warrant or other legal documentation. If a warrant or court order is presented, make sure your hospital or clinic has a trained staff member or administrator who can review the validity of the document, which should be:
Signed by a judge
Contain the address of the premises to be searched
Contain the time period in which it may be executed
Include the date of the search (ensure the time of presentation is during the authorized time period)
Contain disclosure of the scope of a search (is it limited to an individual person, specific documentation, such as I-9 audits, or full access to a physical facility?).
ICE Does Not Override Patient Privacy
The Health Insurance Portability and Accountability Act (HIPAA) privacy law generally prohibits the use or disclosure of personal health information without a patient’s consent, except when required by law. The latest immigration executive order does not override federal HIPAA regulations.
Some HIPAA exceptions, including the permission to disclose information requested by law enforcement officials for law enforcement purposes, allow for otherwise protected health information to be shared under some circumstances, but its release is generally not required. This means that hospitals are generally not obligated to disclose this information but may choose to do so.
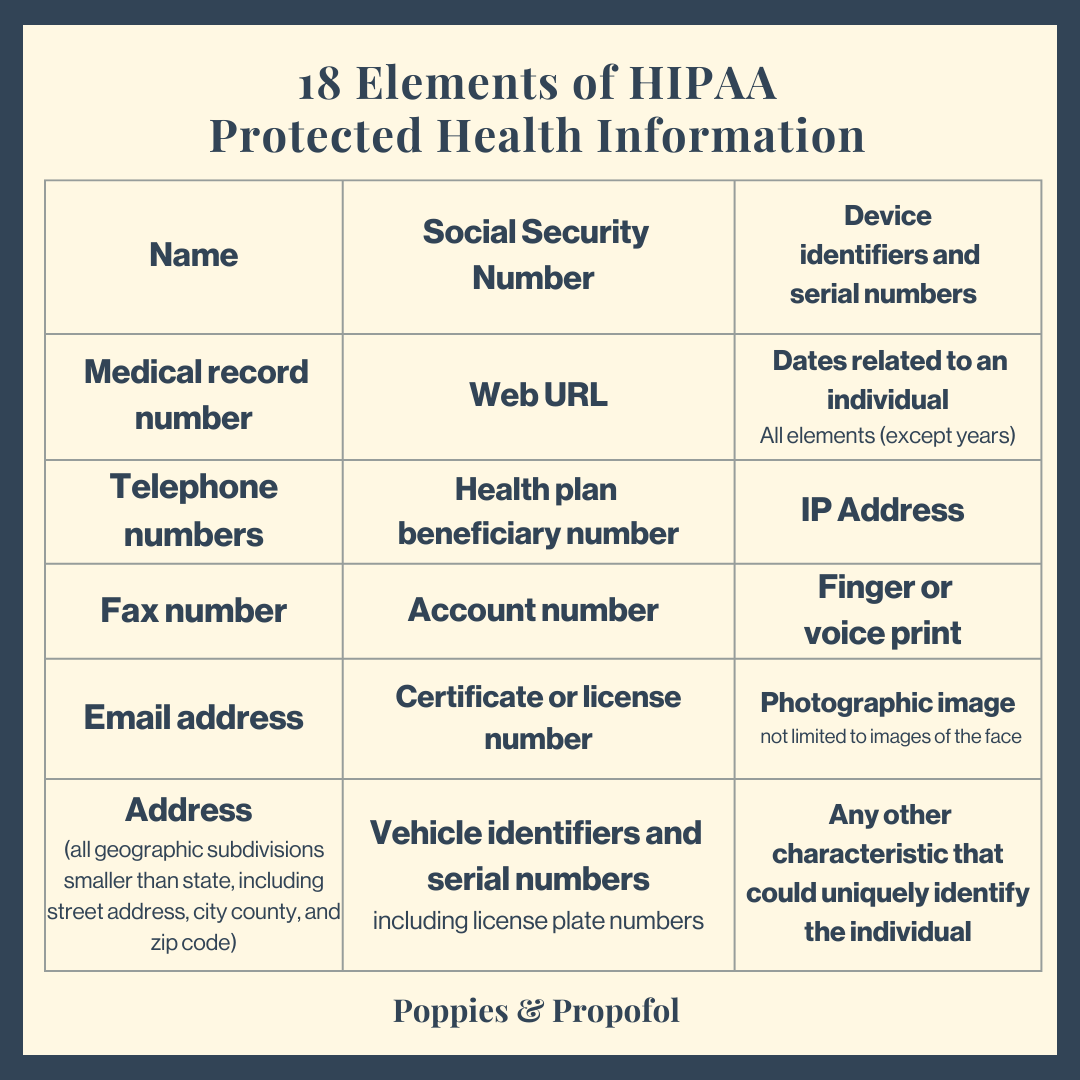
Know the 18 HIPAA Identifiers
If any identifier (or parts of an identifier, such as initials) are included in a communication, the data is “identified.” Without a patient's permission to disclose, disclosure violates patient privacy. For data to be considered “de-identified”, every single one of the 18 HIPAA Identifiers must be removed from the communication. This includes all dates, such as surgery dates, and all photographic images.
When in doubt, remember that last protection: Any other characteristic that could uniquely identify the individual.
14 Tips for Healthcare Workers
It is critical that healthcare workers pause and not rush to comply with law enforcement agents’ requests for access and information. Consider these tips in conjunction with advice from your local legal council and reputable advocacy organizations.
Policies, Notification, and Legal Guidance
Ensure hospital policies regarding law enforcement, including immigration agents, are current, providing healthcare workers with clear guidance.
Find out who you should immediately notify (manager, administrator, or other) when you receive any request by an immigration enforcement officer for access to the healthcare facility, patients, or facility documentation.
Get legal support from your hospital or other trusted legal resource.
Patient Care Comes First
Immigration status should never compromise patient care. Healthcare providers have a duty to provide standard care.
Patient care must be prioritized over the interests and requests of immigration agents.
Healthcare providers have a duty to protect patients’ privacy (HIPAA).
Healthcare providers have a duty to provide emergency and stabilizing care (EMTALA).
When engaging with a person claiming to be an immigration agent:
Like any other hospital visitor, agents do not have a right to be in patient care areas: You can ask agents to leave any care area.
Insist on seeing identification. Make a copy and document their supervisor’s phone number. (ICE and CPB agents are not police officers but may wear uniforms that say “police” or “federal agent” (see image above); officers should also carry identification badges.)
Request officers provide legal documentation for access (warrant, administrative request, or other documentation from the Department of Homeland Security or other federal or state agency.)
Even if the agent has a warrant or other legal authorization, you do not have an obligation to speak with agents or disclose any information.
For any request for information that may compromise the care of any patient, the provider may refuse to disclose or delay any potential disclosure until required to comply with a warrant or order signed by a judge or authorized authority.
Immigrant patients have many rights beyond privacy.
Patient have Patients have a right to remain silent.
Agents do not have the right to search patients or their belongings without consent or probable cause.
Put Patients over Partisanism
Healthcare workers and systems can choose to put patients and their safety above the partisan interests of government officials. Such protections are in alignment with our ethical duty to care for patients.
Yet in this partisan environment, we have to ask:
Will systems show the institutional courage to protect patient privacy in the face of partisan pressure to comply with raids?
Will healthcare workers betray their sacred oath to protect patients?
Will workers who violate patients’ privacy be held accountable by their organizations? By legal systems?
Resources for Healthcare Workers & Systems
Does your hospital need a policy? Or to update an existing policy? Check out these model policies from California:
University of California’s policy “Responding to Immigration Enforcement Issues Involving Patients in UC Health Facilities”
Office of the Attorney General of California. Promoting Safe and Secure Healthcare Access for All: Guidance and Model Policies to Assist California’s Healthcare Facilities in Responding to Immigration Issues. California Department of Justice. December 2024.
It’s important to understand the limited circumstances under which patient information might be released to law enforcement: American Hospital Association (AHA) and National Association of Police Organizations (NAPO). Guidelines for Releasing Patient Information to Law Enforcement. 2018.
Want to better understand your patient’s rights, direct patients to resources, and learn more about advocacy opportunities?
Health Care Providers and Immigration Enforcement: Know Your Rights, Know Your Patients’ Rights. National Immigration Law Center. December 2024. (*note this document was written prior to rescinding of sensitive area guidance)
Check out resources from CASA: Know Your Rights: Learn How to Protect Yourself and Your Family.
CASA also runs a raid tip hotline: 1-888-214-6016. Call to report any ICE activity.
Your Rights Under HIPAA. HHS.gov.
Many of the principles I covered in 2023 about caring for incarcerated patients also apply.
Sources
Statement from a DHS Spokesperson on Directives Expanding Law Enforcement and Ending the Abuse of Humanitarian Parole. DHS.gov. January 21, 2025. (Accessed on January 23, 2025)
Arundel K & Halleman S. Hospitals no longer protected from immigration raids: The U.S. Department of Homeland Security lifted the practice of avoiding immigration enforcement at hospitals. Healthcare Dive. January 21, 2025. (accessed on January 23, 2025)
Artiga S & Ubri P. Living in an Immigrant Family in America: How Fear and Toxic Stress are Affecting Daily Life, Well-Being, & Health. KFF.org December 13, 2017. (Accessed on January 24, 2025)
Boyle P & Weiner S. Bans on abortion and transgender care have criminalized medicine, putting patients and doctors at risk. November 11, 2024. (Accessed on January 24, 2025)
Pillai D & Artiga S. Potential Impacts of New Requirements in Florida and Texas for Hospitals to Request Patient Immigration Status. August 26, 2024. (Accessed on January 24, 2025)
HB 2293, 51st Leg, 1st Sess (Ariz 2013). Bill did not pass.
New law mandates police officers be in every emergency department in state. ABC News. September 30, 2024. (accessed on January 24, 2025)
Schweikart SJ. Should Immigration Status Information Be Considered Protected Health Information? AMA J Ethics. 2019 Jan 1;21(1):E32-37. doi: 10.1001/amajethics.2019.32. PMID: 30672416. (accessed on January 22, 2025)






Helpful advice I will be sharing with my teams at work. I have already seen the “chilling effect” negatively impact immigrant patients, who are now terrified to seek healthcare. Hoping all health systems promote a similar sentiment and expectation to protect patients.